When detected early, surgery and regeneration offer hope, say experts
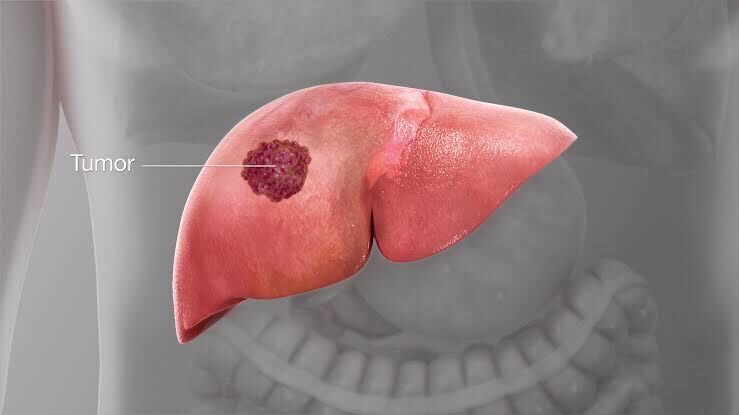
Hyderabad: Liver cancer is rising globally, but what worries experts most is how silently it progresses.
Many people feel fine until the disease has already grown strong. That is where surgery, the only treatment with curative potential, can make a decisive difference.
When tumours are detected early and liver function is still robust, surgeons can remove or replace the diseased portion and offer a real chance at long-term survival. The key challenge is timing: every case is different, and the window to act is often narrow.
When the scalpel can cure: Liver Resection
For tumours limited to part of the liver, surgeons prioritise resection, removing only the affected segment.
Dr RV Raghavendra Rao, Director and Senior Consultant Surgical Gastroenterologist and Liver Transplant Surgeon at Renova NIGL Hospitals, explains, “When cancer is localised, surgery can be curative. The liver has remarkable regenerative ability, and we make full use of that.”
He adds that the priority is always balancing removal with function: “We want to take out the cancer completely but leave the liver capable of sustaining the patient. That balance is critical.”
Advances in laparoscopic and robotic techniques now allow the same goals with smaller incisions and faster recovery.
“Minimally invasive surgery has changed the experience for patients, shorter stays, quicker mobility, and less discomfort,” he says.
When the liver cannot sustain itself: Transplantation
For patients with cirrhosis or multiple tumours, transplantation becomes the stronger option.
“Transplantation gives the patient a new organ and a new chance. It’s not just treating the cancer, it’s treating the liver disease that allowed the cancer to grow,” Dr Rao notes.
But there are systemic hurdles: “We are always racing against time. Organ shortage is real. Eligibility must be decided quickly and precisely.”
Even after surgery, lifelong monitoring is required to prevent recurrence and protect the new liver.
The shift toward precision
Better imaging and planning tools are helping surgeons reduce risk and preserve healthy tissue.
“We are mapping blood flow, tumour depth, and regeneration capacity in detail. The goal is to remove exactly what must go, nothing more.”
This focus keeps more treatment options open if the disease returns.
Beyond the operation theatre: The team effort
Liver cancer care has become a coordinated process involving multiple specialities.
“A single doctor does not treat liver cancer anymore,” Dr Rao says. “Oncologists, radiologists, hepatologists, every voice matters because one decision can change the outcome.”
This approach ensures each case receives a thorough evaluation before landing in the operating room.
Early Detection: The missing link
Dr Rao says the biggest gains will come before the scalpel even appears. “Most patients come late. If they came earlier, a large percentage could be operated on with curative intent.”
“Screening individuals with hepatitis, alcohol-related liver disease, fatty liver, and other risk factors is essential,” he stresses.
Public education, he believes, is now as vital as technology.
Looking ahead
Research is rapidly expanding into targeted therapies and immunotherapies that can shrink tumours before surgery or prevent recurrence later.
“We are entering an era where the biology of the tumour will guide every step,” says Dr Rao. “Personalised treatment is no longer a concept, it’s becoming standard.”
With innovation, early detection, and stronger transplant networks, specialists believe the fight against liver cancer can shift in favour of the patient. “Our purpose is simple,” Dr Rao puts it plainly. “To give every patient the best chance, and to keep pushing that chance higher.”
Source link

